Families and Communities
Flint reminds us that lead poisoning is still very real.
Take action before health and learning suffer.
Signs of childhood lead poisoning are not obvious and there’s no safe level. The only way to know is through a blood test.
Get an answer right away.
Ask your doctor for a simple fingerstick test.
Flint reminds us that lead poisoning is still very real.
Take action before health and learning suffer.
Signs of childhood lead poisoning are not obvious and there’s no safe level. The only way to know is through a blood test.
Get an answer right away.
Ask your doctor for a simple fingerstick test.

Growing children don’t have time to wait.
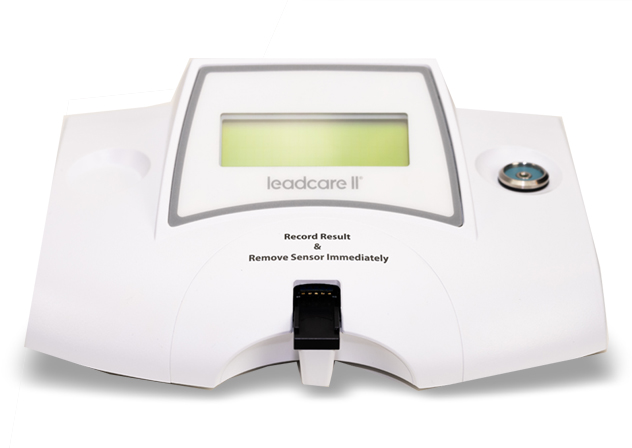
The simple fingerstick (just two drops of blood) for the LeadCare II System is easier than other tests, which require blood drawn from a vein.
Results from the LeadCare II are available on-the-spot, with no extra trips to the lab or doctor’s office. If treatment is needed, your healthcare provider can guide you through the next steps while you are in the office.
Who is at risk for lead exposure?
Children living in or frequently visiting a home built before 1978.
Infants, children and pregnant women consuming water with lead levels in excess of 15 parts per billion.
Recent immigrants, refugees, or foreign adoptees.
Children and pregnant women who use traditional, folk, or ethnic remedies.
Children with a sibling or frequent playmate with elevated blood lead levels.
Families of adults who work with lead. Examples include battery recycling or manufacture, electronics recycling, lead smelting, lead mining, auto repair, shipbuilding, construction, plumbing, and glass manufacture.
1 in 38 US children has an elevated blood lead level

Learn more about the impact of lead exposure
Learn to get started with the LeadCare II System, comply with state and federal requirements, and find answers to frequently asked questions.
Resource Library