Clinicians
Point-of-care lead testing means everybody wins.
3 minutes. 2 drops of blood. 1 visit. Zero loose ends.
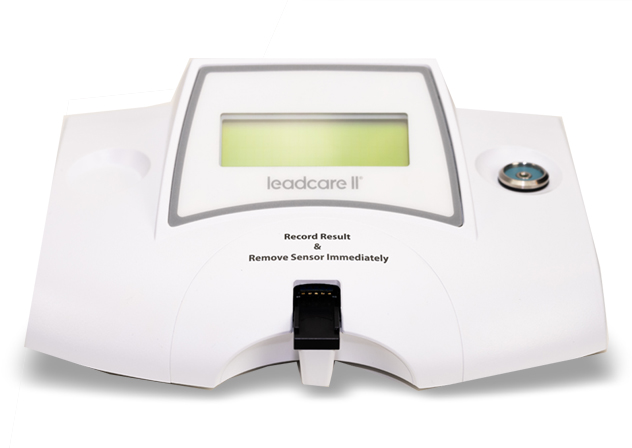
LeadCare® II is the only CLIA-waived, point-of-care lead testing system that makes it possible to test, educate and intervene on-the-spot, in one visit. No need to send patients to an outside lab. No need to re-test due to sample problems at the lab. No risk of losing track of a child who needs treatment.
Point-of-care lead testing means everybody wins.
3 minutes. 2 drops of blood. 1 visit. Zero loose ends.
LeadCare® II is the only CLIA-waived, point-of-care lead testing system that makes it possible to test, educate and intervene on-the-spot, in one visit. No need to send patients to an outside lab. No need to re-test due to sample problems at the lab. No risk of losing track of a child who needs treatment.

Have you found the children at risk in your practice?
1 in 38 U.S. children has harmful blood lead levels. Federal law requires that all Medicaid eligible children be tested at 12 and 24 months and ages 36 to 72 months if they have not previously been tested.
Each state has guidelines or state specific testing requirements for blood lead testing. The American Academy of Pediatrics (AAP) recommends that “children should be tested at least once when they are 2 years of age or, ideally, twice, at 1 and 2 years of age, unless lead exposure can be confidently excluded.”
No safe levels. Evidence continues to grow that blood lead levels as low as 5 ug/dL may impair cognition, with no minimum threshold yet identified.
Early diagnosis helps to quickly address the effects of lead exposure and provides an impetus for lead abatement in homes.
LeadCare II is the only CLIA-waived point-of-care blood lead testing system. Any employee of an office or lab operating under a CLIA Certificate of Waiver can administer the test.
For current pricing and promotions, email us at leadcaresales@meridianbioscience.com or contact your LeadCare II distributor.
Who is at risk for lead exposure?
Children are considered at risk if any of the following are true:
- Child lives in a home built before 1978
- Child has a sibling or frequent playmate with elevated blood lead levels
- Child’s parent or primary caregiver works with lead. Examples include: battery recycling or manufacture, lead smelting, lead mining, auto repair, shipbuilding, construction, plumbing, and glass manufacture
- Child is a recent immigrant, refugee, or foreign adoptee
- Child has a household member who uses traditional, folk, or ethnic remedies or cosmetics or who routinely eats food imported informally (e.g., by a family member)
Lifelong consequences of lead exposure include:
- Six times higher likelihood of having a reading disability
- Seven times more likely to drop out of high school
- Lower scores on tests for math, reading, nonverbal reasoning and short-term memory
- Decline in IQ with every 1.0 μg/dL increase in blood lead
To request more information or to schedule a product demonstration, contact us.
1 in 38 US children has an elevated blood lead level

Support for our customers and patients
Learn to get started with the LeadCare II System, comply with state and federal requirements, and find answers to frequently asked questions.
Resource Library